How Physicians Are Really Paid: Is There a Disconnect Between Value and Volume?
Even though this analysis first circulated a few years ago, the findings remain just as relevant today. RAND and Harvard researchers led by Rachel Reid, MD, MS, published in JAMA confirmed what many in the industry have sensed...despite value-based reimbursement from payers, physician compensation inside health systems remains overwhelmingly volume-driven. Only 9% of primary care and 5% of specialist compensation is tied to value metrics.
Nonetheless, there is a critical nuance worth noting…. the payer-to-health system contract is often completely separate from how health systems and practices compensate their providers.
- RAND Article: "Despite Push to Reward Physicians for Quality and Value, Most Health Systems Base Pay on Volume"
- JAMA Publication: "Physician Compensation Arrangements and Financial Performance Incentives in US Health Systems"
- Thought provoking review of this by Eric Bricker, MD
The Hidden Disconnect
Even when a payer rewards a system for lowering cost or improving quality, those funds may not flow directly to the individual physicians driving that change. Internal compensation formulas often remain built on:
- Work RVUs that reward throughput
- Fixed salaries for coverage stability
- Stipends or call pay for access obligations
This structural lag may explain why most “value-based” arrangements still behave like volume-based engines at the provider and health system level.
Inside the Compensation Cascade
Within a single system, physician pay can vary dramatically across departments and individuals. A cardiologist might be paid by RVUs, a hospitalist by shift, and an imaging physician by stipend… all under the same payer contract.
That complexity makes it difficult to align clinical behavior with system-level value targets.
Mapping the Models
In U.S. health systems, the flow of professional and technical revenue depends on whether care is delivered in an inpatient (bundled under DRG) or outpatient setting. Admitted encounters typically roll the technical component into the hospital DRG, while professional fees are billed separately by the physician group. For outpatient or ED discharges, both professional and technical components are billed independently, aligned to site-of-service fee schedules and governed by revenue cycle responsibilities, payer contracts, and local compliance rules.
As organizations move toward risk-bearing or shared savings models, several compliance and regulatory guardrails must remain top-of-mind.
- Anti-Kickback Statute (AKS), Stark Law, and Fee-Splitting prohibitions continue to shape how compensation structures can be legally designed and distributed.
- Risk adjustment activities require defensible documentation that reflects active monitoring, evaluation, and treatment planning for any new or reaffirmed diagnosis.
- Corporate Practice of Medicine (CPOM), credentialing and scope of practice rules differ by state, defining what physicians, nurses, and other clinicians may perform and bill under supervision or delegation.
- Data privacy and AI governance frameworks are also tightening, particularly where clinical decision support or analytics influence patient care or reimbursement.
These elements make compensation design as much a compliance exercise as an economic one. Even well-intentioned incentive models can create exposure if documentation, credentialing, or governance do not align with regulatory expectations.
Provider Compensation Models
Below is a concise high-level representative summary of 17 physician compensation and revenue integration models, spanning from traditional salary and RVU structures to emerging risk-sharing and joint venture models:
| 1. Hourly Compensation | Description: Fixed hourly rate for time worked Professional Revenue: Not linked to output; revenue retained by employer or hospital Technical Revenue: Retained by the hospital for capital and operating expenses |
| 2. Salary-Based Compensation | Description: Fixed annual salary tied to coverage expectations Professional Revenue: Indirectly influences salary reviews or discretionary bonuses Technical Revenue: Hospital-retained |
| 3. Productivity-Based (RVU) | Description: Pay driven by RVUs generated through procedures and interpretations Professional Revenue: Directly tied to production; incentivizes higher volume Technical Revenue: Hospital-retained unless joint ownership exists |
| 4. Performance-Based (Quality Incentives) | Description: Compensation linked to quality, safety, and satisfaction metrics Professional Revenue: Quality scores factor into bonus pools Technical Revenue: Hospital-retained; may fund quality infrastructure |
| 5. Blended Model | Description: Combines salary, productivity, and quality components Professional Revenue: RVUs and quality metrics define bonus potential Technical Revenue: Retained by hospital, with potential for limited revenue sharing |
| 6. Stipend-Based | Description: Fixed payment for call coverage or defined service obligations Professional Revenue: Usually encompassed in stipend Technical Revenue: Retained by hospital |
| 7. Partnership or Equity-Based | Description: Physicians share ownership of the practice or service line Professional Revenue: Distributed through ownership shares Technical Revenue: Shared if group owns equipment; otherwise hospital-retained |
| 8. Shift-Based with Differential Pay | Description: Variable pay based on timing or coverage intensity (nights, weekends) Professional Revenue: Not directly linked Technical Revenue: Retained by hospital |
| 9. Locum Tenens | Description: Temporary coverage, daily or hourly pay Professional Revenue: Flat rate, not tied to volume Technical Revenue: Retained by hospital or health system |
| 10. Hybrid Models | Description: Custom blend (salary, productivity, and quality) aligned to service goals Professional Revenue: Influenced by procedural billing or population outcomes Technical Revenue: Hospital-retained, with potential sharing for equipment co-ownership or performance agreements |
| 11. Value-Based / Risk-Sharing | Description: Incentives tied to cost containment, outcomes, and total cost of care (eg, ACOs, bundled payments, ACO REACH) Professional Revenue: May include shared savings or downside risk participation Technical Revenue: Shared indirectly through total cost performance Strategic Relevance: Central to payer-provider alignment and CIN sustainability |
| 12. Co-Management Agreements | Description: Physicians compensated for operational oversight of a defined service line (eg, imaging, cath lab) Professional Revenue: Unchanged for clinical work; administrative stipend layered on Technical Revenue: Hospital-retained but optimized through throughput and quality gains Strategic Relevance: Aligns physician engagement in hospital efficiency and compliance |
| 13. Gainsharing / Alignment Incentives | Description: Bonus distribution from hospital cost savings tied to utilization or efficiency metrics Professional Revenue: Supplemental, separate from billing Technical Revenue: Derived from hospital cost reductions or bundled payment reconciliation Strategic Relevance: Bridges physician engagement in cost stewardship |
| 14. Global Budget / Capitation | Description: Fixed PMPM or per-population payment encompassing all or most services Professional Revenue: Patient Panel-based distribution model Technical Revenue: Integrated within capitated rate or shared risk pool Strategic Relevance: Core to VBC models and payer-provider joint ventures |
| 15. Academic / Research & Teaching | Description: Compensation for education, research, or grant-funded work Professional Revenue: Effort-based salary allocations or grant supplements Technical Revenue: Institutional, typically excluded from direct compensation Strategic Relevance: Common in AMCs and hybrid faculty-clinician structures |
| 16. Joint Venture / Service Line Ownership | Description: Shared ownership of imaging centers or outpatient facilities between hospitals and physician groups Professional Revenue: Direct billing plus profit distributions Technical Revenue: Shared based on equity and operating agreements Strategic Relevance: Common in MSO-PC virtual health and diagnostic joint ventures |
| 17. Non-Clinical Incentive Models | Description: Rewards for leadership, innovation, or transformation work (eg, AI deployment, service redesign) Professional Revenue: Project-based or discretionary stipends Technical Revenue: N/A Strategic Relevance: Supports clinician engagement in digital and operational innovation |
Each has distinct implications for how professional and technical revenue flow — and how value truly reaches the front line (or not).
The Foundational Framework Requisite: How Health Care Gets Paid
I often leverage Kevin Quinn's paper, “The 8 Basic Payment Methods in Health Care” to help educate on the building blocks of the current healthcare business models in use and although published in 2015, it remains relevant even a decade later. Thus, before redesigning compensation, it helps to revisit the underlying payment building blocks that shape how money flows through the system. Quinn outlined eight basic payment methods and their derivatives, shown below:
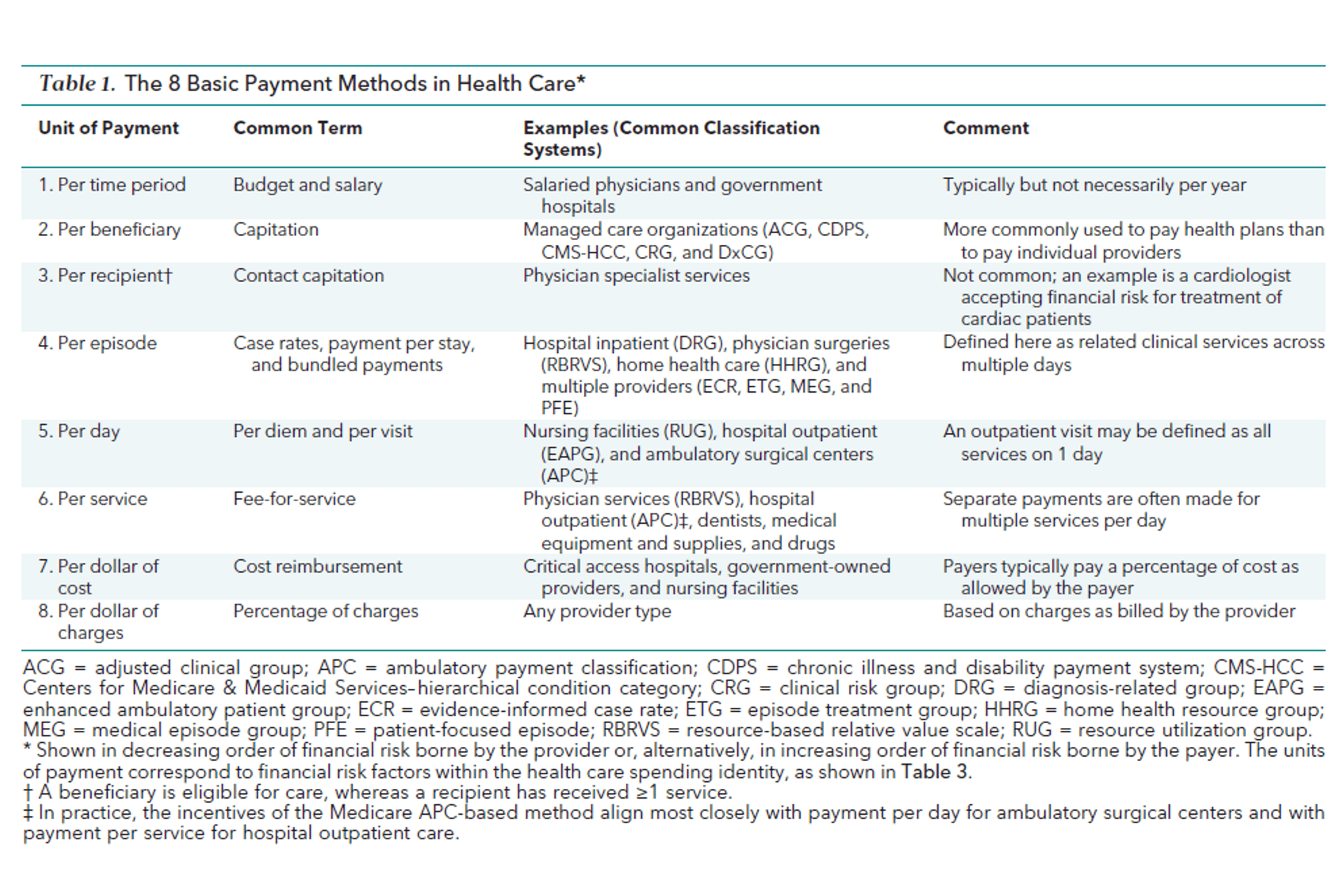
Contemplating Payment Reforms and Implications for Physician Compensation
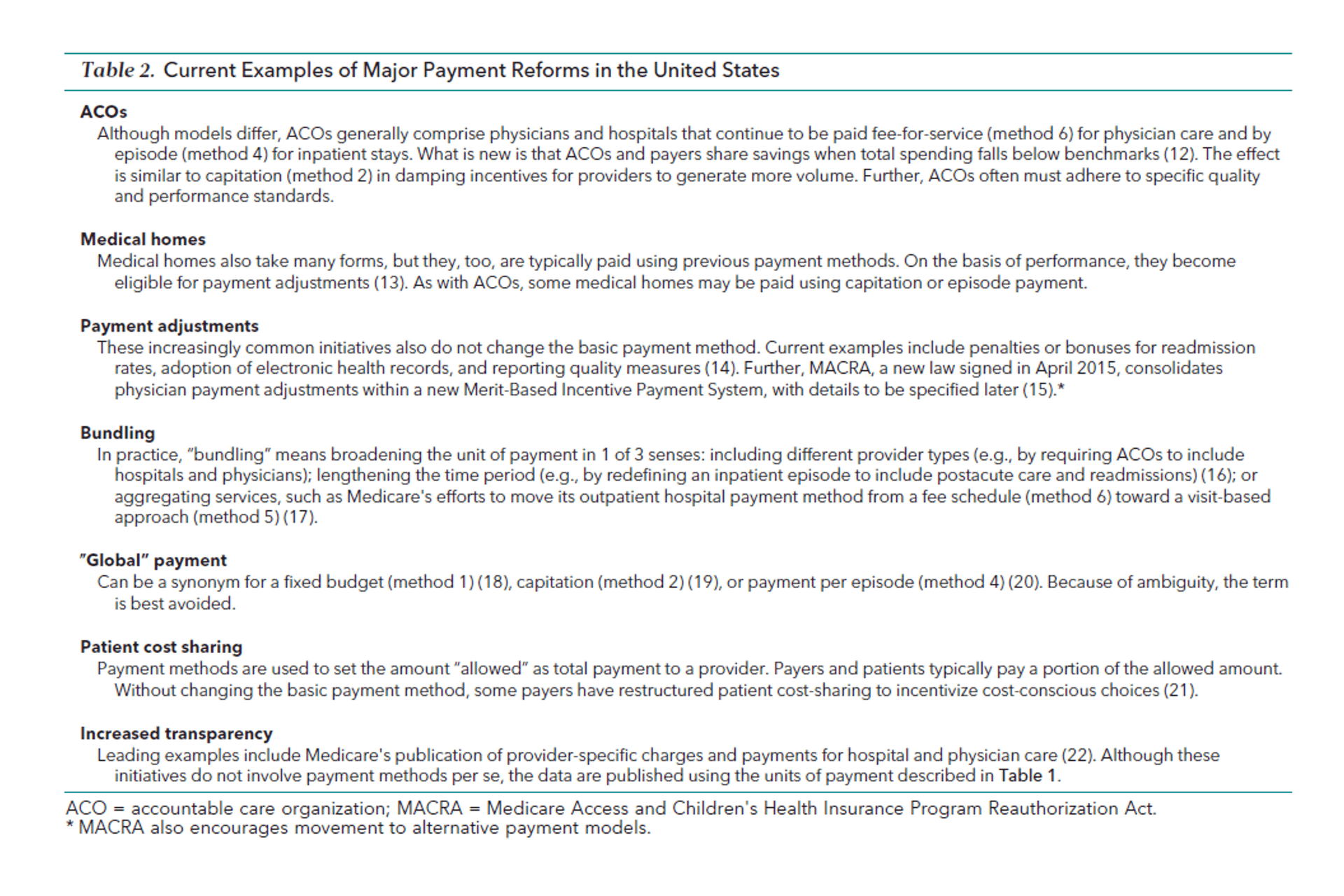
Many payment reforms including ACOs, bundled payments, patient centered medical homes, and shared savings extend these models by linking performance to population outcomes, yet physician compensation has largely lagged behind in adopting corresponding incentive frameworks. Also highlighted in Quinn’s work:
Considerations in the Path Forward
Health systems that aspire to true value-based care must integrate compensation design into their broader contracting, governance, and performance frameworks. Until those incentives align, physicians will continue operating in two economies: one funded by value, another rewarded by volume.
The future of physician alignment will not be decided by payer contracts alone. It will depend deeper business innovation with regard to how health systems choose to translate value into compensation and how transparently they connect clinicians to the outcomes they create.
